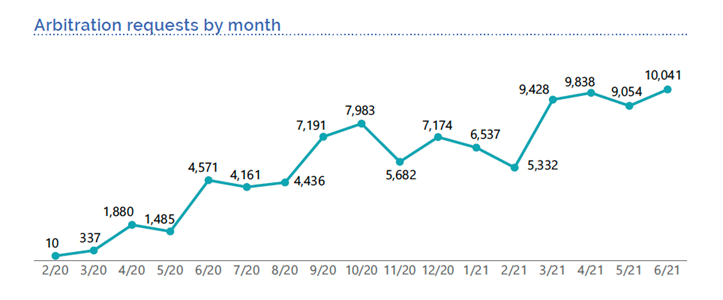
Two years after Texas implemented a new arbitration process for resolving surprise medical bills, the number of arbitration requests have skyrocketed to more than 50,000 requests from January to June 2021, suggesting a costly trend that will leave consumers and employers on the hook for higher health care costs in the future. In a new report, the Texas Department of Insurance reports that “dispute resolution requests received in the first six months of 2021 already exceed the number of requests from 2020” with emergency room physicians responsible for an overwhelming majority of arbitration claims.
Consumer and patient advocates, leading employers, health insurance providers and health policy experts have repeatedly warned against the abuse and misuse of arbitration. Ahead of the Biden Administration’s release of new rules around arbitration, also known as independent dispute resolution, the Texas report provides a warning sign for how arbitration could become a loophole for out-of-network providers and private equity firms to game the system. Highlights from the report are included below:
- Top providers submitting requests for arbitration between January – June 2021:
- Emergency department physicians – 35,172
- Anesthesiologist – 8,238
- Certified registered nurse anesthetist – 1,993
- Radiologist – 1,749
- Surgical assistant – 759
- In total, the fees associated with arbitration in Texas have exceeded $30 million for 2021 alone. Arbitration expenses are covered by the provider or the health insurance plan, much of which will be passed through in the form of higher health care costs for patients and consumers.
To view the impact of arbitration in key states, click here. To learn more about how the Biden Administration can protect patients from abuse of arbitration, click here.
Recent Comments