Out-of-network providers continue to exploit patients at their most vulnerable – even in cases where those patients made the effort to seek in-network care.
- A recent report from Kaiser Family Foundation found that the vast majority (90 percent) of inpatient stays for consumers with employer-sponsored coverage were at in-network facilities. Even when patients were admitted to in-network facilities, 16 percent of these stays resulted in at least one out-of-network charge for medical care.
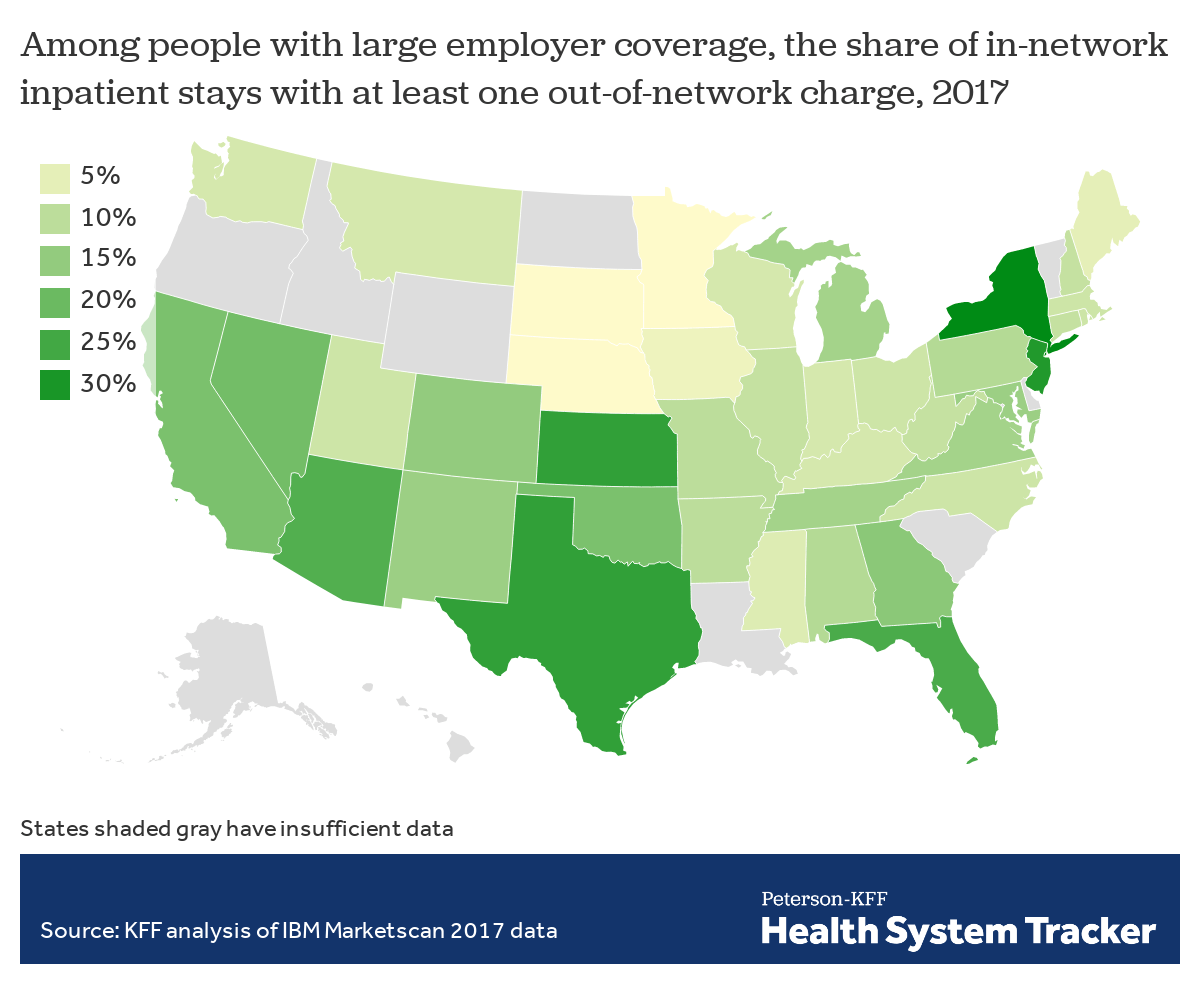
- The problem is even more alarming for patients in New York, New Jersey, Texas and Florida who face a far higher likelihood of receiving an out-of-network bill at an in-network facility.
Patients in urban areas are more likely to face out-of-network charges for inpatient stays than those in rural communities.
- The same Kaiser report found that patients receiving inpatient care in urban areas were somewhat more likely to receive an out-of-network bill compared to those living in rural communities. Sixteen percent of inpatient stays in urban areas result in at least one out-of-network charge, compared to 11 percent of stays in rural areas.
A benchmark based on local, in-network rates would ensure provider reimbursement accurately reflects the cost of providing care in each market while directly addressing the extreme out-of-network outliers who continue to charge unconscionable rates.
- According to research from Yale University, while 50 percent of hospitals have out-of-network billing rates below two percent, 15 percent of hospitals have out-of-network billing rates above 80 percent.
- Data show that in many cases a median, in-network rate would still far exceed the Medicare rate provided for the same service. For example:
- Anesthesiologists are reimbursed a median contracted amount of 344 percent of Medicare;
- Emergency physicians’ average contracted rates are 306 percent of Medicare; and,
- Radiologists’ average contracted rates are 200 percent of Medicare.
Experience in the states show that a benchmark is the best way to expand patient access to care and lower costs for families and employers.
- In California, a year after implementation of the state’s payment benchmark, at least two health plans have seen 5 – 7 percent increases in the percent of ancillary providers they contract with at acute care facilities.
- After Maryland implemented a benchmark for out-of-network charges, there was a related decline in balance billing as a share of out-of-network payments (from 21 percent to less than 10 percent) from 2010 – 2013. Researchers found no evidence that provider participation declined during that time.
- The opposite is true in states like Texas that previously enacted policies to require payments of billed charges similar to arbitration-like models. Today, Texas has some of the most egregious rates of surprising billing in the nation.
Recent Comments