The Problem
Surprise medical bills—also known as “balance billing”—have long been one of the most pressing affordability concerns facing American families. Historically, most states allowed doctors to bill patients for any balance remaining after their health insurance paid its share. These charges were particularly devastating when out-of-network providers—who had no contractual rate agreements with insurers—billed patients for the full cost of care.
Today, with the No Surprises Act in place, patients are protected from most surprise medical bills. But new challenges have emerged. Certain private equity–backed providers and profit-focused intermediaries are now exploiting the law’s arbitration process as a business model to maximize revenue.
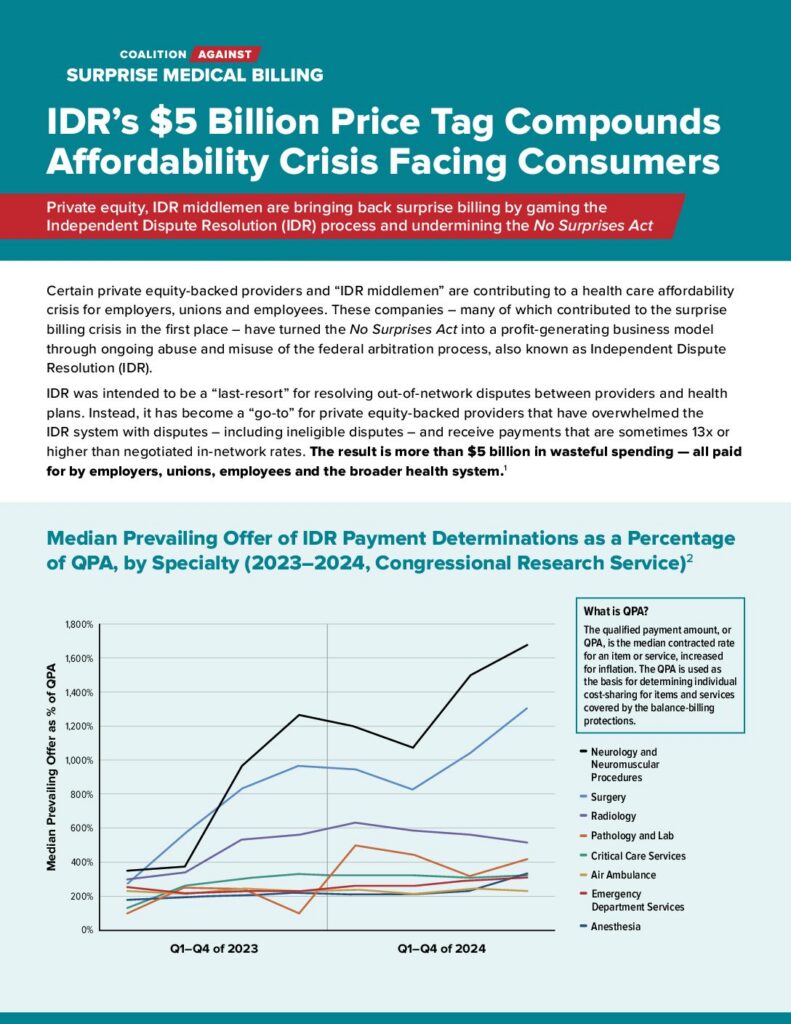
Instead of serving as a last-resort mechanism for payment disputes, the independent dispute resolution (IDR) process has been flooded with claims. Millions of cases have been filed since the law’s passage—far exceeding government projections—many of which are ineligible or inflated. This surge has created costly bottlenecks, slowed down legitimate dispute resolution, and burdened both health plans and employers with unnecessary administrative fees.
What’s more, data show that providers are prevailing more frequently in arbitration, and when they win, their awards are often many times higher than typical in-network or Medicare rates. This not only drives up direct costs for health plans but also raises premiums and out-of-pocket expenses for American families. Meanwhile, IDR entities are not required to provide full explanations of their decisions, and the law lacks a clear appeals process—leaving limited accountability or oversight.
Latest News
A +$2,000 Bill for a Runny Nose? Nutex Health’s Charges Show What Went Wrong With IDR
It’s no surprise that private equity-backed providers—including Nutex Health—have co-opted the No Surprises Act’s (NSA) IDR process into their go-to profit center. It’s the reason why private equity-backed championed arbitration as their “solution” to the surprise...
By the Numbers: How Private Equity and IDR Middlemen Abuse the No Surprises Act and Cost Americans Billions
Congress and the President enacted the No Surprises Act to protect patients from outrageous medical bills and create a balanced, predictable system for resolving payment disputes between health plans and providers, while lowering costs. Instead, some private...
Private Equity Plays Both Sides of the No Surprises Act — and Patients Are Paying the Price
When Congress passed the No Surprises Act, the goal was clear: protect patients from unexpected out-of-network medical bills and lower costs for employees and employers. But a new analysis from the Private Equity Stakeholder Project (PESP) finds that private equity is...